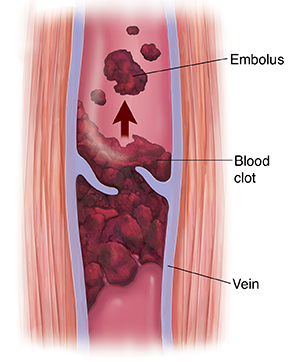
Deep Vein Thrombosis (DVT)
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in a deep vein. This happens most often in the leg. It can also happen in the arms or other parts of the body. A part of the clot called an embolus can break off and travel to the lungs. When this happens, it’s called a pulmonary embolism (PE). PE is a medical emergency. It can cut off blood flow and lead to death. Both DVT and PE are closely related. Together, they are often referred to by the term venous thromboembolism.
Risk factors for DVT
Anything that slows blood flow, injures the lining of a vein, or increases blood clotting can make you more likely to have DVT. This includes:
-
Long periods without movement (such as when sitting for many hours at a time or when recovering from major surgery or illness).
-
Estrogen (female hormone) therapy, such as hormone replacement therapy (HRT) or birth control pills.
-
A fractured hip or leg.
-
Major surgery or joint replacement.
-
Major trauma or a spinal cord injury.
-
Cancer.
-
Family history of DVT.
-
Excess weight or obesity.
-
Smoking.
-
Older age.
-
Past history of a DVT.
-
Inherited clotting disorders.
Symptoms
DVT does not always cause symptoms. When symptoms do occur, they may appear around the site of the DVT, such as in the leg. Possible symptoms include:
-
Swelling.
-
Pain.
-
Warmth.
-
Redness.
-
Tenderness.
Home care
-
You were likely prescribed blood thinners (anticoagulants). They may be given as pills (oral) or shots (injections). Follow all instructions when using these medicines. Note: Don't take blood thinners with other medicines, herbal remedies, or supplements without talking to your health care provider first. Certain medicines or products can affect how blood thinners work.
-
Follow your provider’s instructions about activity and rest.
-
If support or compression stockings are prescribed, wear them as directed. These may help improve blood flow in the legs.
-
When sitting or lying down, move your ankles, toes, and knees often. This may also help improve blood flow in the legs.
Follow-up care
Follow up with your health care provider, or as advised. If imaging tests were done, they may need further review by a provider. You will be told of any new findings that may affect your care.
When to get medical advice
Contact your health care provider right away if you have:
-
New or increased swelling, pain, soreness, warmth, or redness in the leg, arm, or other area.
-
Blood in the urine.
-
Bleeding with bowel movements.
Call 911
Call 911 if you have:
-
Bleeding from the nose, the gums, a cut, or the vagina.
-
Heavy or uncontrolled bleeding.
-
Trouble breathing.
-
Chest pain or discomfort that gets worse with deep breathing or coughing.
-
Coughing (may cough up blood).
-
Fast heartbeat.
-
Sweating.
-
Anxiety.
-
Lightheadedness, dizziness, or fainting.
Online Medical Reviewer:
Heather M Trevino BSN RNC
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Sravani Chintapalli
Date Last Reviewed:
1/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.